Utilizing Language Translation Devices Breaking Down Communication Barriers on Your Travels


As technology continues to advance, the field of translation and localization is also seeing significant changes. In the coming years, we can expect to see a number of developments that will improve the accuracy and efficiency of language translation, making it easier for people and businesses to communicate across borders.
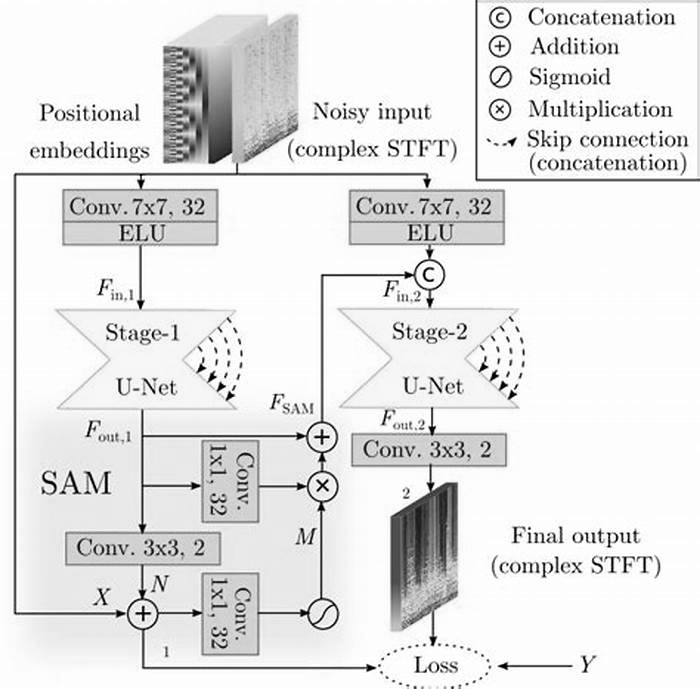
One of the most exciting developments in the field of translation is the use of neural machine translation (NMT), like Google Translate. NMT is a form of artificial intelligence (AI) that is able to learn the intricacies of a particular language and apply that knowledge to translations. This has led to a significant improvement in the quality of translations, particularly for less common languages.
Another area where we can expect to see advancements is in the use of natural language processing (NLP) to aid in localization. NLP is a field of AI that deals with the interaction between computers and human language. By using NLP techniques, like ChatGPT, software can be made to understand and respond to language in a more human-like way. This will make localization more accurate and efficient, as software will be able to understand the nuances and idioms of different languages and cultures.
With the increasing use of virtual and augmented reality technology, we can expect to see more demand for the translation of multimedia content. The ability to translate and localize video, audio and other multimedia content will become increasingly important as this technology becomes more prevalent. This also present new challenges and possibilities for localization, as translation engine will need to deal with idiomatic language, context, and tone.
We can also expect to see an increase in the use of crowdsourcing for translation and localization. By leveraging the power of the crowd, companies will be able to quickly and cost-effectively translate and localize their content into multiple languages. This has already been used in some companies, but will become more mainstream in the future as the approach improves and becomes more accessible.
In conclusion, the field of translation and localization is constantly evolving, and we can expect to see a number of exciting advancements in the coming years. The use of neural machine translation, natural language processing, and multimedia localization will improve the accuracy and efficiency of language translation. Additionally, the use of crowdsourcing will make it more cost-effective for businesses to communicate across borders. These developments will have far-reaching implications for industries such as e-commerce, education, entertainment, and many more, breaking down language barriers and making the world a more connected place.
Evidence-based approaches to breaking down language barriers
LANGUAGE BARRIERS between nurses and patients increasingly affect nursing practice, regardless of where care is delivered. In the United States, a language other than English is now spoken at home in one of five households, the highest level since just after World War I.1 Patients with limited English skills are referred to as patients with limited English proficiency (LEP).
This article provides background information about language barriers between nurses and patients and some strategies for addressing these gaps. After detailing how these barriers affect patient outcomes, practice-based strategies are offered to improve outcomes and reduce readmissions. Although the article doesnt address barriers to communicating with patients with hearing loss, many of the same principles apply to these patients.
Sources of spoken language barriers
Globalization means more people move around the world for work and educational opportunities.2 When people migrate, they tend to follow immigrant networks and start recreating communities in their new country.3 People also migrate and become refugees due to wars and civil conflicts.3 Countries that accept these refugees place them in communities where they can recover from the trauma of their migration experiences while seeking work and learning about their new country.
Structured refugee resettlement has been going on in the United States since after World War II.4 With the exception of Native Americans, just about everyone in this country is descended from immigrants. When patients have a language barrier, its often related to when they migrated to the United States.
Perhaps unsurprisingly, the largest group of migrants in the last 30 years speaks Spanish.
5With only 5% of U.S. nurses identifying as Hispanic or Latino, its very common for patients in this group to encounter a language barrier.
6(No publicly available record of language skills of U.S. nurses exists.)
Mandarin and Cantonese Chinese speakers are the next largest group.
1Theyre also underrepresented in nursing.
7The number of Russian-speaking people in the United States is growing quickly. For many Russian-speaking patients, however, Russian is their second or third language. In many countries under Soviet rule in the latter half of the 20th century, people continued to speak their original languages as well as Russian. With the dissolution of the Soviet Union, their preferred language might be the language of their home country.
8
In some parts of the United States, some older immigrants still face a language barrier. For example, many Italians who migrated to the United States in the early 1900s never developed English language skills and may still need interpreter services.9 Language demographics depends on whos moved into your organizations service area.
As people age, some may lose skills in their second language due to how the brain changes with aging.10 Even those who developed strong fluency in English as adults could lose those skills if they have significant age-related neurologic events. Some of these older adults may end up needing interpreter services.
Another trend involves adults who migrated to the United States and then brought their parents over to join the family.11 Although the adult children who brought their parents to the United States may speak English well, their parents may not speak well enough to communicate effectively with a healthcare provider.
How migration dynamics affects nurses
Patients with language barriers change how nurses work and organize care for patients. These changes are needed not only to meet communication needs for the patient, but also for legal reasons. In 1964, the U.S. Civil Rights Act helped ensure that a lack of English language skills wouldnt be a source of discrimination.12,13 U.S. law requires that healthcare organizations provide interpreter services to patients with LEP.14 New regulations implemented as part of the Affordable Care Act place new restrictions on the use of family members and validating language skills of health workers.15
Much evidence shows how language barriers impact patient outcomes and healthcare delivery. (See Evidence-based impact of language barriers on patient outcomes.) Patients with LEP have longer lengths of stay than English-speaking patients, even if they have a higher socioeconomic status.16-18 They also have a higher risk for 30-day readmission, by as much as 25%.18,19 Most of the other outcomes listed in the table are outcomes sensitive to nursing practice.
Evidence-based impact of language barriers on patient outcomes
| Outcome | |
|---|---|
| Length of stay if interpreter isnt used at admission or discharge | (3 days) |
| 30-day readmissions (among certain chronic diseases) | risk (15%-25%) |
| Central line-associated bloodstream infections | risk |
| Falls | risk |
| Surgical site infections | risk |
| Pressure injuries | risk |
| Surgery delays | risk |
| Medication management (for example, adherence, understanding discharge instructions) | risk |
| Preventive screening | chance |
| Access to the healthcare system | chance |
How nurses and other healthcare providers respond to the communication needs of patients with LEP also has a significant impact on patient satisfaction, with effective use of interpreter services or bilingual healthcare professionals contributing to higher patient satisfaction ratings.20-26
A closer look at medical interpreters
Aside from facilitating communication between patients and healthcare providers, medical interpreters can also serve as cultural brokers.27-30 The medical interpreter helps bridge the cultural divide between patients and clinicians. Their translation process ensures that what a nurse says is delivered not only with technical accuracy, but also with culturally specific phrasing. Nurses can assess the quality of medical interpreters cultural brokerage by observing how the patient responds to the interpreter through his or her body language.
Medical interpreters have a professional code of ethics, and theyre required to comply with it when performing their roles.31 Theyre bound by the same patient confidentiality requirements as every other healthcare team member.31
Most interpreters hired by healthcare organizations have undergone some kind of medical interpreter training because healthcare has its own language.32 According to the National Council on Interpreting in Health Care, no minimum number of course hours is required for interpreter training at this time, but it recommends that programs adhere to its curriculum standards, which it developed in 2011.33 Implementing a course that meets the standards usually requires a minimum of 40 hours of study and successful live demonstration of the ability to interpret a medical encounter. Participants receive a certificate after theyve completed a course. They can then take a national exam to become a board-certified medical interpreter.34 Board certification is voluntary at this time.
Improving quality of care and outcomes
How can nurses help improve patient outcomes? These evidence-based strategies can help nurses better organize their care to improve outcomes. These will also help nurses meet the Joint Commission requirements for bridging language barriers.
Use the organizations interpreter resources.
This isnt optional. Interpreter resources typically include in-person interpreters employed by an organization, in-person interpreters contracted through external agencies, and telephone- or technology-based interpreter services. (See 10 tips for working effectively with an in-person medical interpreter.)
10 tips for working effectively with an in-person medical interpreter
For an in-person interpreter, call the interpreter service and specify the language needed and about how much time the interpretation will take.
When the interpreter arrives, introduce yourself and provide a brief report on the work needed and a brief patient history.
Greet the patient and introduce the interpreter. Explain to the patient what will happen, and let the patient know that he or she can ask the interpreter anything, even if its not the main reason for the interpretation. Then begin the activity.
*When working with the interpreter and patient, communicate directly with the patient. Resist the temptation to talk or look at the interpreter, unless you need clarification of something he or she said.
Speak in shorter sentences than normal. Doing so makes it easier for the interpreter to remember the sentence and improves the translations accuracy.
*If the interpreter appears confused about something youve said, ask the interpreter if clarification or rephrasing is needed to improve interpretation quality for the patient.
*Try not to interrupt the interpreter when he or she is translating the patients reply. Guessing what the patient is about to say may not always be right, and some cultures perceive interruptions as very rude behavior.
*If the interpreter seems to be taking a long time to translate for the patient, it may mean that he or she is trying to phrase it in a way that will be best received by the patient. Conversely, if an interpreter simply translates, for example, Yes, to something the patient took a long time to say, that might be an indication of poor translation quality. Make sure the interpreter interprets patients responses completely. Dont accept a yes or no when the patient gave a lot of information, even when youre in a hurry.
When the encounter finishes, ask the patient if he or she needs anything else while the interpreter is there. Many patients have more needs, and often the interpreter encounter has made them feel comfortable enough to express them.
*After leaving the room with the interpreter, review the encounter to ensure both interpreter and nurse ended up on the same page. The interpreter may also have some cultural insights to share that can help with care planning.
*These steps also apply to telephone or video interpretation.
Some organizations deal with language barriers all the time and have excellent resources. They may have an interpreter services department to manage the demand for language interpretation services. Some locations have experience with certain language groups needing translation and need interpretation for only a few languages. Now, however, many healthcare organizations are seeing more diversity and have a greater need for interpreters. Most organizations begin with interpreter phone services and, if the demand becomes high enough, begin employing full-time interpreters.
Telephone interpretation can work if implemented well. According to Tuot et al., a good telephone interpretation session requires minimal waiting time for the phone interpreter, good sound quality so everyone can hear clearly, and an outcome in which both patient and provider obtain the information needed.35
Nonetheless, both nurses and patients have reported problems with interpretation quality and have expressed dislike for the depersonalization of the patient encounter when using the interpreter phone.20,36-39 When no other option is available, however, telephone interpreter services are best to bridge the language barrier. New options with live video interpretation are also coming onto the market and may replace telephone interpreters.
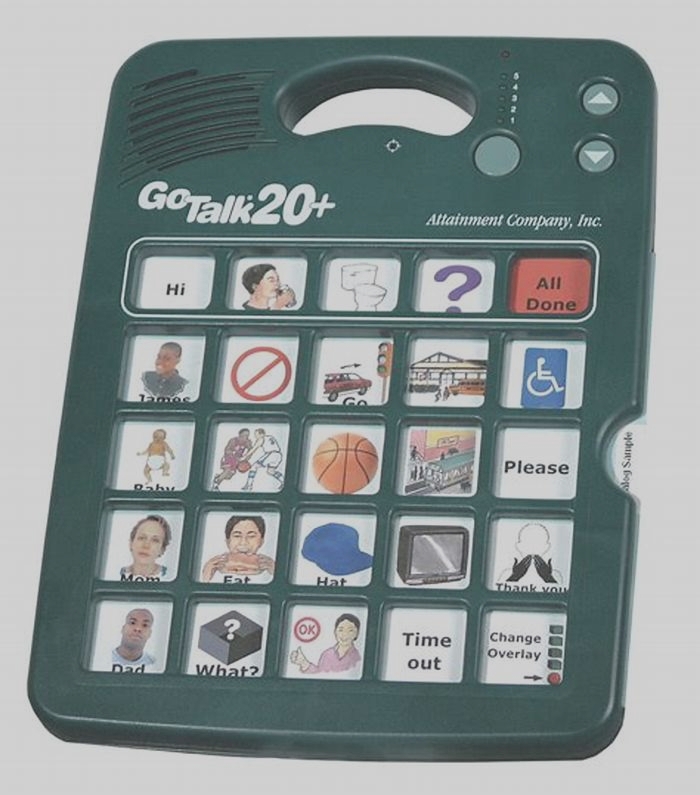
Inappropriate interpreter use, including nonvalidated translation apps on a nurses smart phone, puts the organization at legal risk, as discussed below. Many apps for interpretation are available for smartphones, but their accuracy can be poor and most arent compliant with the Health Insurance Portability and Accountability Act (HIPAA). The quality of translation they provide is rarely evaluated systematically or using rigorous approaches. Many of these apps are also designed for translating only basic sentences, such as how to order dinner when traveling. Most computer programs dont yet have the sophistication needed to translate the language of healthcare. Use only those apps sanctioned by your employer because those have received a thorough internal review and are HIPAA-compliant.
As a general rule, family members, especially children under 18, shouldnt serve as interpreters, except under extenuating circumstances such as an immediate threat to life.40,41 Using a family member to interpret increases the risk that something wont be translated correctly. For instance, a family member may not feel comfortable conveying some sensitive types of information to the patient, such as about sexual health, substance abuse, or a terminal diagnosis. Using a family member also increases the risk of medical errors.35 Depending on the situation, it may also violate patient confidentiality protocols. Err on the side of caution and comply with the law: Dont use family members for interpretation.
Use care when other staff provides interpretation.
Staff members who speak the same language as the patient are another common resource for interpretation, but this practice has its own set of risks. Use coworkers with other language skills appropriately, but only when necessary. The Agency for Healthcare Research and Quality (AHRQ) has developed guidelines for how to better utilize staff with language skills.27 According to the evidence, choosing a nurse or other healthcare professional who speaks the patients language and whos had his or her language skills professionally evaluated by a language assessment expert is best.32
Unlicensed assistive personnel or housekeeping staff members, who are commonly asked to interpret, may not have the medical vocabulary needed to accurately translate for the patient and family. If they become certified as medical interpreters or the organization assesses their language skills, however, they can then be used to translate.
Organizations that are implementing AHRQs guidelines use name badges that designate the staff members language skills. Those employees have had a formal language skills assessment, understand medical terminology in the languages they speak, and speak the language well enough to safely communicate with patients and families.27
Every time you ask professional staff members to interpret, you take them away from their own patients and add to their overall patient case load.30,39,42-44 Consider developing an agreement for the patient-care unit so nurses with other-than-English language skills, with their permission, can be assigned to language-matching patients. Even if this means the staff member doesnt have a geographically efficient assignment, it will help to streamline his or her work.
Document use of medical interpreter services.
Documenting interpreter use is just as important as documenting wound care or any other clinical intervention. Document not only when an interpreter was used but also the type of interpretation. For example, state whether it was at admission or discharge, or for informed consent or patient teaching. Then document whether the interpretation was done by a medical interpreter on staff by telephone, and the interpreters name, or with a computer. In some cases, depending on the organizations policy, the interpreter will be required to document the encounter as well. The interpreter will include information such as the patients unique identifier, time and duration of the encounter, and any other information required by the organization.
When a nurse has to rely on a staff member to interpret, either because no human interpreters were available or because of technologic difficulties, documenting the decision making behind that choice will help to protect the nurse as well. Showing every effort was made to adhere to organizational policy means the nurse has done whats legally required.
Time interpreter use strategically.
Research shows that the three critical times when nurses should use interpreters are at admission, during patient teaching, and at discharge. Using interpreters at these times decreases the risks of medical errors and hospital readmissions.18,36,45-47
How will it help? During admission, using an interpreter will provide more accurate baseline information. That, in turn, will help the healthcare team create a more accurate plan of care. An interpreter can also help nurses tailor patient teaching to the needs of patients and their educational level. At discharge, having an interpreter present is equally critical, even if it delays discharge by a few hours. A good patient discharge process with an interpreter will decrease the risk that patients will be readmitted because they didnt understand how to take their medications or other discharge instructions.18,47
An idea for a clinical ladder project, for nurses working in places with such a promotion system, is to have discharge instructions and patient-education materials translated into languages spoken by many patients. Bilingual discharge instructions will also ensure that when patients are referred for home health services, home healthcare nurses who dont speak their language can also read the discharge instructions. The more resources that can be used for teaching and facilitating discharge for patients with LEP, the less likely they are to be readmitted or visit the ED.18,47
Prioritize patient understanding of medication management.
Medication adherence is complex when patients speak English, but even more so when patients have LEP.48,49 First, medications may have different names in other countries, even in other English-speaking countries, and may require translation. Second, whenever possible, medication instructions should be in the preferred language of the patient. Remember that even when someone speaks some English, he or she may not be able to read it. An oral review of medications using teach-back techniques will help promote adherence, reduce readmissions related to failure to take new medications or understand changes to the old regimen, and help with care coordination with community-based providers.27